In addition to the psychological comorbidities associated with Autism Spectrum Disorder, studies have shown that there is also a variety of medical comorbidities associated with ASD. Immune dysregulation is perhaps the most widespread of these and has been shown to contribute to an array of immuno-inflammatory diseases,  including lupus, MS, celiac disease, inflammatory bowel disease, and eczema, to name a few. The same studies have also provided evidence to suggest that the chronic inflammation in the perinatal environment can contribute to the development of ASD, thus leading the child to exhibit both ASD and immune dysregulation. Therefore, understanding the root of these comorbid disorders is critical to developing treatment and prevention mechanisms for both.
including lupus, MS, celiac disease, inflammatory bowel disease, and eczema, to name a few. The same studies have also provided evidence to suggest that the chronic inflammation in the perinatal environment can contribute to the development of ASD, thus leading the child to exhibit both ASD and immune dysregulation. Therefore, understanding the root of these comorbid disorders is critical to developing treatment and prevention mechanisms for both.
As diagnosis and awareness of neurological disorders have increased in the last decade, so has research into the root causes of these disorders. With this research has come a vast increase in knowledge and thus an expansion of treatment options that alleviate symptoms of both ASD and the 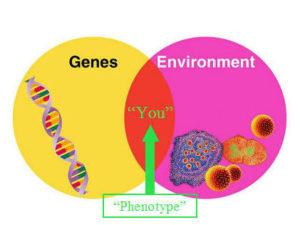 comorbidity in question. It is important to understand that ASD is caused by a combination of environmental and genetic factors, and that environmental signals can influence gene expression. A study from UC Davis explored this idea in depth, and found that “a specific set of antibodies to fetal brain proteins” was found in blood samples taken from mothers of children with ASD. Subsequently, the European Journal of Pediatrics linked these antibodies to “chronic neurological inflammation and immune dysregulation leading to upregulation of inflammatory cytokines in the ASD brain.” With this knowledge, recent studies have explored the possibility of prevention strategies for mothers in addition to treatment strategies that can be practiced post-partum.
comorbidity in question. It is important to understand that ASD is caused by a combination of environmental and genetic factors, and that environmental signals can influence gene expression. A study from UC Davis explored this idea in depth, and found that “a specific set of antibodies to fetal brain proteins” was found in blood samples taken from mothers of children with ASD. Subsequently, the European Journal of Pediatrics linked these antibodies to “chronic neurological inflammation and immune dysregulation leading to upregulation of inflammatory cytokines in the ASD brain.” With this knowledge, recent studies have explored the possibility of prevention strategies for mothers in addition to treatment strategies that can be practiced post-partum.
The National Autism Association has released a detailed article on the topic of medical comorbidities in autism, with a specific focus on inflammatory issues associated with autistic children. In addition, the article focuses on 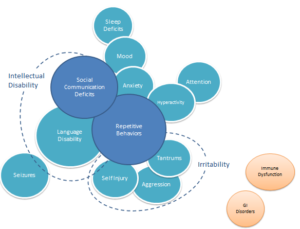 specific cases in which the treatment of an inflammatory disease leads to alleviation of ASD symptoms including repetitive behavior, agitation, and anxiety.
specific cases in which the treatment of an inflammatory disease leads to alleviation of ASD symptoms including repetitive behavior, agitation, and anxiety.
One powerful example referenced a 5-year-old boy, Steven, with severe ASD symptoms including hyperactivity, aggression, and obstinance. Upon medical examination, Steven was found to have tonsillar enlargement and raised inflammatory markers. He was started on a course of co-amoxiclav for strep throat, and within three weeks Steven’s ASD symptoms had significantly improved. This is only one of many examples across a variety of studies in which treatment of an inflammatory medical condition increased social and cognitive function in ASD children.
While it is critical to acknowledge the existence of and the treatment options for medical comorbidities of autism, it is just as important to  recognize the importance of approaching treatment from the neurodiversity perspective. While medications and other interventions can resolve physical issues and alleviate some of the negative symptoms of ASD, we should not approach affected children with the attitude that we need to “cure” their autism. Rather, we should aim to help ASD children thrive and grow in the most comfortable, safe manner possible while allowing them to use their diverse minds in full.
recognize the importance of approaching treatment from the neurodiversity perspective. While medications and other interventions can resolve physical issues and alleviate some of the negative symptoms of ASD, we should not approach affected children with the attitude that we need to “cure” their autism. Rather, we should aim to help ASD children thrive and grow in the most comfortable, safe manner possible while allowing them to use their diverse minds in full.
Sources
http://nationalautismassociation.org/pdf/MedicalComorbiditiesinASD2013.pdf
https://asdresearchinitiative.wordpress.com/2012/09/20/autism-and-the-immune-system-special-bilbo/
https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-016-0712-5
Speak Your Mind